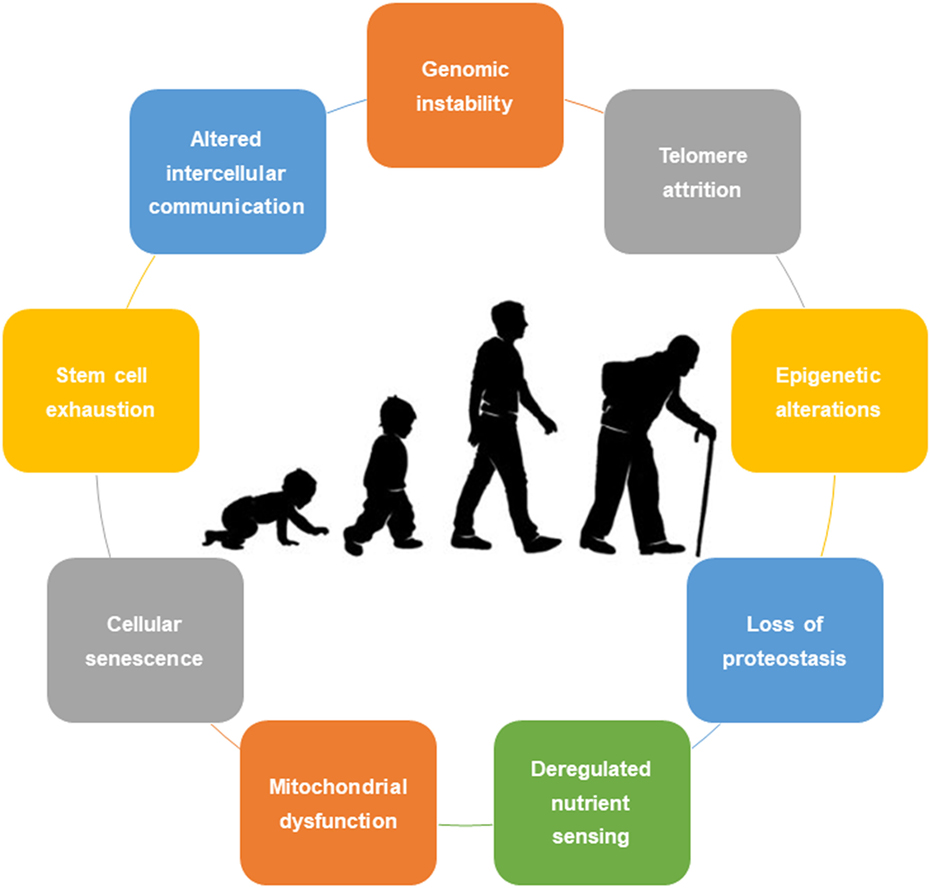
Scientists now believe that our lifestyle choices—especially weight—could be accelerating the aging process deep in our cells. Researchers reveal that obesity significantly speeds up epigenetic aging, but there’s a promising twist: a specific diet may help reverse this biological time warp.
A recent study published in nutrients, explored whether obesity accelerates biological aging and if a Very Low-Calorie Ketogenic Diet (VLCKD) can reverse it. They used DNA-based “epigenetic clocks” to measure biological age and found that people with obesity were aging quicker, but shed years off their biological age after the diet.
It’s a bold claim—but does the science really hold up?
We help health orgs and researchers communicate insights clearly — reach out if you want to collaborate!
A recent study published in nutrients, explored whether obesity accelerates biological aging and if a Very Low-Calorie Ketogenic Diet (VLCKD) can reverse it. They used DNA-based “epigenetic clocks” to measure biological age and found that people with obesity were aging quicker, but shed years off their biological age after the diet.
It’s a bold claim—but does the science really hold up?
We help health orgs and researchers communicate insights clearly — reach out if you want to collaborate!
🧪Study Summary
This study explored the relationship between obesity and biological aging, measured through DNA methylation using three epigenetic clocks (Horvath, Hannum, and Levine).
The results were striking:
- Individuals with obesity showed significantly higher biological age (DNAmAge) compared to their normal-weight peers—an average acceleration of +4.4 years.
- In contrast, normal-weight individuals had a deceleration of -3.1 years, indicating slower aging.
- The degree of age acceleration was strongly correlated with BMI across all models.
To test whether this process could be reversed, the researchers implemented a Very Low-Calorie Ketogenic Diet (VLCKD) for patients with obesity. Results showed:
- After 30 days of VLCKD, participants experienced an average epigenetic age reversal of −6.1 years, which persisted through 180 days.
- This deceleration in aging was strongly associated with ketone levels (β-hydroxybutyrate), BMI reduction, and improvements in metabolic health markers (glucose, insulin, cholesterol, leptin, etc.).
🔍 Critical Review: Methodology Under the Microscope
1. What Was the Study Trying to Figure Out?
The researchers were curious—does obesity speed up biological aging? And can a Very Low-Calorie Ketogenic Diet (VLCKD) slow that down or maybe even reverse it?
- To their credit, they weren’t claiming cause-and-effect. This was more about spotting patterns or associations.
⚠️The issue? The title and how they framed the study sound like they’re promising a reversal of aging—which is a pretty big leap for this kind of design. - On the plus side, using epigenetic clocks to measure biological age is smart and relevant—it’s one of the better tools we have to explore this question.
Remarks: The research question is fair for a first pass. But the language they use might give people the wrong impression about what the study can actually prove.
2. How Was the Study Designed?
They took a two-part approach:
- A cross-sectional group compared people with and without obesity.
- A longitudinal group tracked people with obesity on a VLCKD over six months.
The comparison helps spot differences in aging markers tied to obesity.
Following people on the diet gives clues about how their biological age might shift over time.
⚠️ The catch? The diet group had only 10 participants—that’s a tiny sample to draw solid conclusions.
⚠️ Even more importantly, there was no control group. So we don’t know if any improvements were from the diet—or just natural changes, exercise, or even placebo effects.
⚠️ Plus, there was a noticeable age gap between the groups. The diet group was older, and since aging itself affects these markers, that kind of mismatch can muddy the waters.
Remarks: The study offers a nice exploratory peek, but small numbers, no controls, and mismatched ages make the findings more of a conversation starter than a final word.
⚠️ Issue: Lack of Information on Obesity’s Causes
Why it matters: Obesity isn’t a one-size-fits-all condition. There are tons of factors that can contribute to it, including:
- Genetics
- Hormonal issues like PCOS or hypothyroidism
- Mental health struggles or stress
- Lifestyle factors (e.g., diet and exercise)
- Socioeconomic factors and environmental influences
These different causes can affect how our bodies age at a genetic level. For example, someone who is obese because of stress might have different epigenetic changes than someone whose obesity is linked to a genetic predisposition or poor diet.
⚠️ Issue: Missing Physical Activity Data
What’s missing: The study doesn’t mention physical activity at all—either in how they assessed participants or in how they analyzed the data. This is a big oversight, especially when we’re talking about obesity and aging.
🏃 Why it matters: Exercise can influence both obesity and epigenetic aging. Regular physical activity can:
- Improve metabolism even without weight loss
- Impact DNA methylation (which is tied to aging)
- Slow down the process of epigenetic aging
Without knowing whether participants were active or sedentary, it’s hard to say if the VLCKD diet alone was responsible for any changes in biological age. If some participants were really active and others weren’t, that could mess up the results.
Remarks : The study didn’t account for physical activity, a key factor that affects both metabolic health and epigenetic aging, which could have skewed the results and made it hard to know whether the observed effects were truly due to the diet or other lifestyle factors.
📈 How This Study Could’ve Been Stronger
Let’s be real—this study had some good ideas, but a few tweaks could’ve really boosted its credibility, especially if we’re talking about whether the diet actually made a difference.
1. No Control Group? That’s a Problem.
One of the biggest gaps? There was no control group. To really know if the VLCKD was doing anything special, we need a similar group of people with obesity who didn’t follow the diet. They could’ve either stuck to a standard low-calorie plan or just continued their usual routine.
2. Small Sample Size = Big Limitations
With only 10 people in the diet group, it’s hard to draw any solid conclusions. A larger group would’ve given the findings more weight. Ideally, they should’ve run a power analysis ahead of time to figure out how many participants they’d actually need to detect real, meaningful changes.
3. Age Differences Were a Bit Off
The folks in the diet group were quite a bit older than those in the comparison group (we’re talking ~49 vs ~36 years). That’s a big deal when you’re studying aging. Aging itself can change epigenetic markers, so we can’t ignore those age gaps. Ideally, all groups should’ve been in a similar age range, say within five years of each other.
💡 Why that matters:
Matching ages helps make sure the effects you’re seeing are from the intervention, not just from people being at different stages in life. Also, the study skipped out on including older adults—yet, that’s a group where the obesity-aging link is especially important. After all, obesity peaks around age 43 for men and 41.9 for women.
4. Understanding the Roots of Obesity
- Assess the causes of obesity up front:
They could’ve collected more detailed medical and lifestyle information, like metabolic panels, hormone tests, diet habits, and stress levels, to get a clearer picture of what’s driving each participant’s obesity. - Look at subtypes of obesity:
They could have divided participants into groups based on whether their obesity was “metabolically healthy” or “unhealthy” to see if the effects on epigenetic aging were different across these types. - Control for other factors:
Using statistical models to account for things like insulin resistance, stress hormones, or inflammation could’ve helped separate the impact of obesity itself from other factors affecting aging.📌 In a nutshell:
To make stronger claims, the study needed a well-matched control group, a bigger sample size backed by power calculations, and tighter age and demographic consistency across participants. And honestly? Including older adults would’ve made the findings a lot more relevant to real-world aging and obesity trends.
📊 3. How Was the Data Collected?
Let’s give credit where it’s due—this study used some solid, science-backed methods for gathering data.
- They used standardized and validated procedures to collect methylation data, like Infinium arrays and GenomeStudio software. That’s a gold-standard move in this field.
- They also collected anthropometric data and fasting blood samples, which helps reduce measurement errors and keeps things consistent.
- Additionally, they didn’t just eyeball aging—they used well-established epigenetic clocks like Horvath, Hannum, and Levine. Good call.
But there are a few concerns…
⚠️ Some of the information—like supplement use or medication history—was self-reported, which always opens the door to recall bias. People don’t always remember (or report) things accurately.
⚠️ And the diet itself was delivered through a commercial program (the PNK® method), which isn’t super transparent. If other researchers wanted to replicate the study, they’d need the exact protocol—and it’s not clear if that’s even publicly available.
Remarks: The data collection process was strong overall, but some parts (like self-reporting and proprietary diet methods) could use more transparency to make replication easier.
📈 4. How Did They Analyze the Data?
On the stats side, they made some smart choices.
- They used AgeAccel, which is a solid way to measure biological aging beyond just someone’s calendar age.
- Paired t-tests and repeated measures ANOVA were used to analyze changes over time and compare groups—these are appropriate for the data they had.
- They also used Holm–Šídák correction for multiple comparisons, which is great because it helps avoid false positives.
But here’s where things could’ve been better…
⚠️ They leaned on Spearman correlations for some associations, which is fine for non-parametric data—but they didn’t adjust for confounders like age, sex, or baseline health status. That’s a missed opportunity, especially in a study on aging and obesity.
⚠️ And let’s not forget: their sample size was tiny. That means some effects might’ve been missed (hello, Type II errors), or the ones they found might not hold up in a larger group.
Remarks: The stats were mostly well-chosen, but the lack of confounder control and the small sample size put a cap on how confident we can be in the results.
⚠️ 2. Analytical Issues & Interpretive Concerns: Let’s Talk About the Fine Print
Alright, so the study does a solid job using modern tools to explore how a ketogenic diet might impact biological aging in people with obesity. But once you dig into the details, a few analytical red flags pop up. Let’s unpack them in plain English.
🔄 A. Correlation Isn’t Causation—Even if It Sounds Like It
Yes, they found some interesting relationships—like how higher ketone levels (specifically β-hydroxybutyrate or β-OHB) were associated with slower epigenetic aging. Sounds exciting, right?
But here’s the catch: correlation doesn’t mean causation. Just because two things move together doesn’t mean one caused the other.
Take this line from the study:
“This finding suggests that the presence of ketone bodies… may be associated with the observed deceleration in epigenetic aging.”
That “may be associated with” phrasing sounds cautious, but if repeated throughout, it can easily be misunderstood as “this caused that.” Especially when the study doesn’t consider other possible explanations—like whether participants also improved their sleep, reduced stress, or made other healthy changes while dieting. Any of those could be influencing biological aging too.
⚖️ B. Confounding Factors Left Out
Here’s where things get a little shaky. The analysis doesn’t adjust for some pretty important variables that could influence both obesity and biological aging, like:
- Existing metabolic conditions (e.g., insulin resistance)
- Medications they might be on
- How physically active they were
- Socioeconomic status and environment
Ignoring these means we can’t really isolate the effects of the diet itself. Maybe people who benefitted the most were already healthier or more active to begin with. Without controlling for that, it’s hard to tell what’s actually driving the results.
🌍 C. Who Does This Apply To?
The study focused only on adults with obesity—and didn’t give much detail about their demographics (like age ranges, ethnic backgrounds, or geographic location). That matters a lot.
So, while the findings are intriguing, they may not apply to:
- People without obesity
- Younger individuals
- Folks from different ethnic or metabolic backgrounds
Bottom line: what works for this group might not work the same way for everyone else.
Final Thoughts: A Solid Start, But Some Gaps
This study definitely pushes the conversation forward about how diet might affect biological aging—but we need to be cautious about how we interpret the findings.
✅ The analytical framework is strong
🚧 But:
- Correlations are a starting point, not a conclusion
- Confounding factors matter
- Generalizability is limited
- Data visuals need full transparency
If future research builds on this with bigger, more diverse samples and better control for external factors, we’ll get closer to truly understanding how dietary interventions like VLCKD influence our biological clocks.
We help health orgs and researchers communicate insights clearly — reach out if you want to collaborate!
Leave a Reply